Exclusive Tips
Sharing what we’ve learned has also been at the heart of what we do. It has enabled us and our clients to learn and grow. It is our hope that the information in Exclusive Tips section helps to inspire you.
How to Increase the Bond Strength of
Zirconia Based Restorations
Zirconia based restorations cannot be acid etched due to their lack of silica and glass, so sandblasting is the preferred surface-roughening method.
Here are some suggested methods to treat zirconia based restorations prior to bonding to improve restoration retention.
Method 1: If Sandblasting (Micro-Etching) Is available
Step 1. Sandblasted with 50 µm Al2O3 particles from a distance of 10 mm perpendicular
to the specimen surface at a pressure of 2.5 bar for 15 s.
Step 2. Coat zirconia surface with Z-PRIME Plus (Bisco Canada 1-800-667-8811) or
Monobond Plus (Ivoclar Vivadent Canada 1-800-263-8182) and allowed to air dry
Step 3. Cement with Preferred Dual Cure Resin Cement

Method 2: If Sandblasting (Micro-Etching) Is Not available
Step 1. Clean zirconia surface with ZirClean Restoration Cleaner (Bisco Canada
1-800-667-8811) or Ivoclean (Ivoclar Vivadent Canada 1-800-263-8182)
Step 2. Coat zirconia surface with Z-PRIME Plus (Bisco Canada 1-800-667-8811) or
Monobond Plus (Ivoclar Vivadent Canada 1-800-263-8182) and allowed to air dry
Step 3. Cement with Preferred Dual Cure Resin Cement


Helping our clients achieve the very best clinical outcomes, is just another way we are,
“Working Harder and Smarter for your Practice!”
Klausz Implant Tip
How to avoid food traps around implant restorations
When a natural tooth is lost and an implant placed, there is usually some type of bone loss which causes the tissue in the papilla region to recede. This in turn creates a space below the natural contact areas of teeth (Figure 1). More prevalent in the posterior quadrants, these areas can’t be closed with the implant restoration as they fall into an undercut from the crown’s path of insertion (Figure 2). The best way to avoid creating these potential food traps is by adjusting the contact areas of the natural teeth prior to taking the implant fixture impression. By reducing the enamel from the height of contour, the gingival embrasure below the contact will decrease in size (Figures 3 & 4). Looking for this potential problem at the onset can save quite a bit of time as well as discomfort for the patient.

Figure 1

Figure 2

Figure 3

Figure 4
Make Abutment Insertion a Snap with a Custom Orientation Jig
Implant abutments fabricated in the dental laboratory, whether modified stock or custom, need to be placed consistently in the same orientation. When the case is completed and sent to the dentist’s office for final insertion, this orientation needs to be transferred from the stone cast to the implant intra-orally. To do this, a “Custom Orientation Jig” should be fabricated. These jigs are made with low shrinkage, pattern resin. They should fit snugly around the core of the abutment and the lateral extensions should rest on the adjacent teeth. They can be placed on the abutment while it is still seated on the model and taken from the model to the mouth (Figures 1, 2, 3, 4).

Figure 1

Figure 2

Figure 3

Figure 4
Accuracy Made Simple With a Small Amount of Wax
The Closed Tray Impression Technique for taking implant level impressions has become very popular over the years. Its simplified approach has given it the advantage over the other method of using an open tray procedure.
Many of the closed tray impression copings have hexes or stars on their tops for the screwdrivers to engage (Figure 1). These openings can lead to a situation where an inaccuracy can be incorporated into the overall impression technique.
Light bodied impression material will flow into these tiny areas leaving a positive interference in the bottom of the impression where the coping needs to reseat. This makes it impossible to reseat the impression copings fully. The result is a final restoration which is dramatically high in occlusion. The solution is to place orthodontic or boxing wax into these spaces on top of the implant transfer copings prior to taking the impression (Figure 2). By neatly filling the opening and not leaving gross amounts of wax on the impression coping heads, the impression copings will fully seat back into the impression.
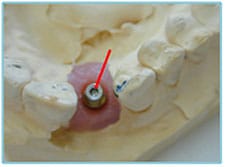
Figure 1

Figure 2
Many patients with complete dentures have, over the years lost, what is referred to as “Vertical Dimension“. When trying to determine how much to re-open the bite, there is a simple and quick test that can be performed that allows us to maintain an average amount of freeway space required for patient comfort. With the patient sitting up straight, with his/her oral muscles in a relaxed state, measure the distance between two points on the patient’s face; for example, the base of the nose and a mark on the chin. This will approximate the vertical dimension the patient requires for adequate freeway space.
Now, have the patient occlude with the dentures in place and measure the distance once again. From the differences in these two measurements we can determine if and by how much the new dentures will need to open the bite. This information can easily be related to the laboratory on the prescription.
The Klausz Modified Denture Technique
Developed to Save You Time and Money in 4 Easy Steps
Over the last five decades, we have developed and perfected our own technique that has greatly enhanced the success of our clients’ complete denture cases. We call it our “Modified Denture Technique“. With this technique, we utilize the patient’s existing complete dentures as a guide to the fabrication of their new dentures.
The concept of the denture technique stems from creating new dentures that improve fit, function and aesthetics, while at the same time maintaining as many similarities to the old set of dentures as possible. The procedure, as an added bonus, requires fewer appointments and provides for a reduced laboratory fee, as the need for custom trays and bite blocks are eliminated.
Step 1: The denture bases are assessed and wash reline impressions are taken.
Step 2: Determine if the vertical dimension needs adjusting to allow for the proper amount of freeway space.
Step 3: A centric occlusion bite is now done with a semi-rigid bite material.
Step 4: In the lab, both arch impressions are poured and mounted onto an articulator with an anterior pin. The original dentures are cleaned and depending on the proximity of the dental office to the dental laboratory, the dentures can even be returned on the same day.
In the lab, the teeth are set up in wax and are returned several days later to the office for a try in. Once the set up has been approved, final processing, trimming and polishing is done, and the completed dentures are ready for insertion.
Replacing worn, complete dentures does not have to be a complex procedure, providing that we make use of the information provided to us from the patient’s original dentures.

Step 1

Step 2

Step 3
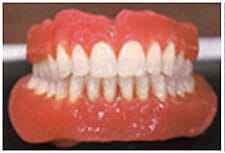
Step 4
Prepare For Success….With Flexible Clearance Tabs


Interproximal Clearance

Occlusal Clearance
We would like to make it easier for our clients to ensure they are creating sufficient occlusal and interproximal tooth preparation clearance for today’s more aesthetic restorations. We have come across a very simple and inexpensive product known as Flexible Clearance Tabs,
Each colour coded Flexible Clearance Tab is made to a specific thickness and is used like a feeler gauge to check preparation dimensions. The tabs are available in three thicknesses, from 1mm pink tabs (Kerr PN 004-006), 1.5mm green tabs (Kerr PN 004-007) to the 2.0mm blue tabs (Kerr PN 004-008). When the tab is drawn between a prepared tooth and its opposing occlusal surface or adjacent tooth, it will verify whether or not adequate clearance has been achieved.
If the tab resists being drawn through the space, there is less clearance than the thickness of the tab. By marking the tab with a Sharpie marker and testing the clearance, the ink will mark the tooth where more occlusal reduction is needed.
We would be pleased to provide you with a complimentary sample package for you to see for yourself how simple and effective these little tabs can be. If you would like to purchase Flexible Clearance Tabs, they are available through your regular dental sundries dealer.
Tips for use:

1. Trim the Tabs
If the tab is too wide to achieve an accurate reading

2. Mark the Tab
Use a sharpie marker to mark the tip of the tab

3. Position the tab
Measure the space between the prep and opposing

4. Results
The sharpie ink left on the prep reveals the reduction
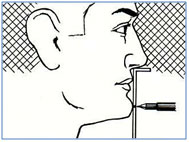
Taking Records for Mandibular Advancement Appliances
such as the Panthera D-SAD Using a George Gauge
Type of Impression

Bite Registration
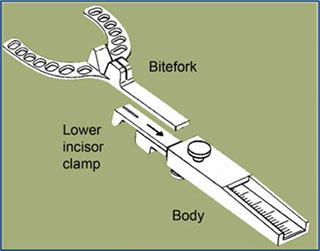
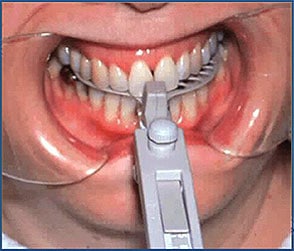
The George Gauge allows the clinician to capture a protrusive bite registration and vertical opening of the mandible while eliminating guesswork. It’s an easy to use tool which provides an extremely accurate way of recording a protrusive bite registration for all Mandibular Advancement Appliances.
Panthera recommends you take the bite registration in full (maximum) protrusion.
First place the George Gauge (without the bite fork) in the patient’s mouth. Center the lower incisor notch over the lower anterior teeth. Cinch up the lower incisor clamp to firmly grip these teeth, and tighten the lower thumb screw to secure.
Remove the instrument from the mouth. Insert the bite fork into the body of the gauge, and slide it until the indicator end is at the 0 point on the millimeter scale (this will give an end-to-end bite position). It is recommended that you use the shorter 2 mm bite fork. You can modify the groove, with a carbide bur, where the maxillary central incisors would go, if the teeth are not straight and do not fit into the groove.
Return the instrument to the mouth with the lower incisor notch centered over the lower midline. Instruct the patient to close into the upper incisor notch with the midline indicator between the central incisors.
Have the patient slide into maximum protrusion. You may wish to have the patient practice this a few times prior to locking the George Gauge into position, as the first few times the patient may not know exactly what you are looking for and will not advance their mandible fully.
When you feel the patient understands the position their mandible should be in (in maximum protrusion), with the George Gauge in place, have them slide their mandible into maximum protrusion and lock the bite fork in position by tightening the thumb screw. Now remove the George Gauge from the mouth, liberally inject your bite registration material on the bite fork, and then reinsert the George Gauge ensuring the mandibular and maxillary central incisors fit back into the grooves, as they were prior to the bite registration material application.
With the George Gauge inserted, you may wish to inject additional bite registration material along the buccal surfaces of the posterior teeth to ensure a solid registration is captured.
By taking the bite registration in maximum protrusion, any lateral deviations with be captured. The software used to design the Panthera D-SAD will automatically place the mandible back to a 60% protrusion prior to fabricating the device.
Some dentists may choose alternate types of bite registrations, such as a Phonetic Bite or a 60% Maximum Protrusive Bite. The appliances can be fabricated to whatever bite you prefer. Please specify on the lab prescription what type of bite registration you have provided. It is not necessary to record the range of movement from retrusion to protrusion.
If the patient’s maxillary and mandibular midlines do not correspond, it is not necessary to have them shift their mandible to fit their maxillary incisors into the bite fork groove. It is better to record their bite in a non-manipulated protrusive movement. It doesn’t matter if the patient’s mandible deviates to the left or right in full protrusive. It is recommended that the bite registration be taken in maximum protrusion to record these deviations if they do exist.
If you are looking for a high quality bite registration material, that does not slump or run when using a George Gauge, we recommend Acu-Flow Bite Registration Material. We currently are a distributor of Acu-Flow Bite Registration Material. You can find more information on our website at the link below.
https://www.klauszdentallab.com/dental-products/#accuflow
Also, it is advisable when prescribing mandibular advancement devises, such as the Panthera D-SAD, that a Bite Repositioning Appliance be made. You can find more information on these on our website at the link below.
https://www.klauszdentallab.com/orthotics-sleep/#bitereposition
The George Gauge can be purchased through our laboratory or you can “try before you buy” as we have a George Gauge that we will gladly loan to you.

Crowns to Fit Clasps Without Sending The Denture To The Lab
A technique for fabricating a new crown that fits an existing
RPD clasp without forcing the patient to surrender their partial
When a tooth under a partial denture requires crowning, the dentist traditionally picks up the prosthesis in a full arch transfer impression and sends it to the laboratory. This allows the technician to use the clasps as a guide when creating the crown contour. For most patients, going dentureless (even for a few days) is unpleasant.
The following technique uses a Blu-Mousse Super-Fast index to register the clasp-tooth-relationship. This allows the technician or dentist to create an accurate template of the clasp. As a result, the patient never has to surrender the prosthesis.

PART 1: How to make a clasp/tooth index using Blu-Mousse Super-Fast material.
1. Prepare the tooth and take the working impression as usual.
2. Insert the RPD in the mouth and assure that it is properly positioned (Figure 1).
3. Inject Blu-Mousse Super-Fast over the preparation. Continue expressing material until the clasps and occlusal rests are completely covered (Figure 2).
4. 30 seconds later remove the RPD with the Blu-Mousse blob attached (Figure 3).
5. Using a blade, carefully trim away the Blu-Mousse until the outer surfaces of the clasps and rests are exposed (Figure 4). Cut away any additional material that prevents the Blu-Mousse index from being removed (Figure 5).
6. Remove the index from the partial denture by pushing it in an apical direction (Figures 6 & 7), temporize the preparation, and send the patient home wearing the partial denture.
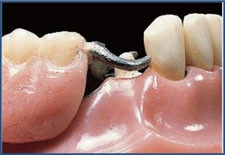
Figure 1

Figure 2

Figure 3

Figure 4

Figure 5

Figure 6

Figure 7
PART 2: In the lab we create a clasp template using pattern resin.
PART 2: In the lab we create a clasp template using pattern resin (Figure 8 & 9). When the patient presents for crown cementation, the new crown fits the RPD with few (if any) adjustments (Figure 10), even though the technician never saw the actual partial denture.

Figure 8

Figure 9

Figure 10
Always looking for ways to improve the quality of our work is just another way we are,
“Working Harder and Smarter for your Practice!”
VISIT US
Mailing Address
40 Kodiak Crescent, Units 11-12
Toronto, ON, M3J 3G5
HOURS OF OPERATION
Monday: 7:30am - 5:30pm
Tuesday: 7:30am - 5:30pm
Wednesday: 7:30am - 5:30pm
Thursday: 7:30am - 5:30pm
Friday: 7:30am - 5:30pm
Saturday: Closed
Sunday: Closed